Independent pharmacies are continually being pressured by PBMs through high DIR fees, clawbacks, and low reimbursement rates.
Getting into the long-term care space through Medical at Home and GeriMed’s ComboMed pharmacy program is a way for retail pharmacies to avoid DIR fees and avail themselves of the benefits offered by the organization.
RxSafe recently presented a webinar that talks about the specifics of the program and how retail pharmacies can participate.
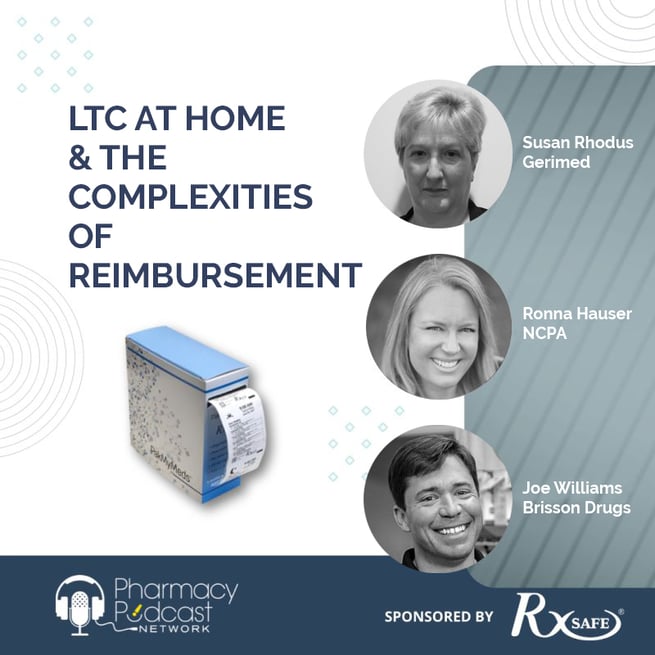
Here are some of the highlights from the webinar “LTC at Home & the Complexities of Reimbursement” with guests:
- Susan Rhodus, Senior VP of Contracts & Advocacy at GeriMed
- Ronna Hauser, Senior Vice President for Policy & Affairs at NCPA
- Joe Williams, Pharmacy Owner and Operations Consultant at Brisson Drugs
Todd Eury of the Pharmacy Podcast Network moderated the discussion.
Todd Eury: How do community pharmacies grow the home care business side of their pharmacies? What services through community pharmacy are primary to home bound patients? Where do we start to define this?
Ronna Hauser: NCPA has been advocating for several years, primarily in front of CMS, to recognize these services. These are services that are akin to long-term care pharmacy services that are currently provided, for instance, to Medicare part D patients in a skilled nursing facility who need an institutionalized level of care. So, what we have done and how we've really advocated for this level of service and this level of care in the home setting is taken that core set of services that pharmacies are required to provide to long term care residents in the Part D program.
We've taken that core set of services and kind of overlaid them into the Medical at Home model and said, “You know, pharmacies providing these services need to be able to provide all of the services they would as if they were contracted as part of a Part D, long-term care network minus the emergency kit.” That would be one obvious thing that you're not going to have to provide in a home setting that you would otherwise in a skilled setting, but at a minimum, those are the services that should be provided. And that every pharmacy participating at this level of service should be able to provide
Todd Eury: How do we get our community pharmacies paid for the ‘low hanging fruit’ services that they're probably already providing that are very similar to traditional long-term care pharmacy services?
Susan Rhodus: Well, that's a big piece of what we've been working at on at GeriMed. We've been trying to get PBMs to recognize that these are important services, and it shouldn't matter where the patient lives, it's what services that that patient needs. And I definitely want to emphasize the word “needs”, because I think sometimes people think of this as more as convenience. It's not the person [Joe Smith] who lives in Florida and drives around in his golf cart. He wants to golf every day. He'd rather do that than go to his community pharmacy to pick up his medications. If he can drive a golf cart, he can drive a car and he can go pick his medications up. So, he would not qualify for being one of these patients.

But if ‘Mrs. Jones’ has got cognitive impairment, she has her spouse taking care of her and making sure she gets her meds every day. And she's not able to leave her home alone because she has this cognitive impairment. She's not able to do that. And she has to have someone helping her with her activities of daily living.
At least two of those, then she could potentially be a candidate. And I think these services that are really important to start out with are things like special packaging, to make sure that they have the packaging done, just like they do in long term care, whether that's a bingo card or a packaging that's a strip packaging set up based on the time of the day that you take your medications. It's 24/7 service that you can get ahold of a pharmacist and get treatment sent to you. It is IV medications, and we have a lot of our pharmacies go, “Well, I don't have an IV hood. I can't miss IVs.“
Well, that's okay. You just need to be able to contract and do a subcontract with someone who can, and it could be a hospital in your area who could potentially provide those services, or it could be a home infusion pharmacy that you contract with to be able to get those in case you need those, the chances of somebody in a home really needing those IV services on a regular basis is probably going to be pretty slim to none.
With 71 million baby boomers, we know that community pharmacies have to be ready, prepared, and also get paid for the services that they can deliver to these home bound patients that don't want to move out of their home.
— Todd Eury, The Pharmacy Podcast Network
But you have to have the ability to do that. That's part of the CMS guidelines for Medicare Part D for long term care.
So those are the things that you really need to do, and then also delivery. And it's not delivery of a bunch of vials in a white bag that you knock on a door and hand it to the person who enters it. That's not the idea. The idea is to provide way more services than that, including things like syncing up their medications and calling the caregiver and the prescribers on a regular basis to make sure that they have what they need for doing medication management, doing reconciliation if they do go to the hospital to make sure they're on the right medications, all of those things are very important in addition to providing dispensing services.
So now, how do you get paid? Well, that's the big gorilla in the room – it’s trying to get paid.
We have been successful with a couple of small PBMs to get payment from them. But it's two very small ones. We're kind of using them as precedent that somebody's already done this. And we've been talking a lot to the Medicare advantage side and also discussing with a coalition to try and get people to really understand that this is an important piece and that there are savings for the healthcare system, as well as providing better care to these patients and providing a mechanism for pharmacies to make more money. All of those things are really important.
Todd Eury: What are the criteria for CMS or PBMs in determining that a patient is a candidate for specific home care services?
Ronna Hauser: This is something that we're still working through. I don't think there is a defined set of criteria that we've all landed on yet. As I mentioned, we recently formed a coalition and we're having ongoing discussion about the best set of criteria. I would say for our discussions to date, most of the dialogue was around ways that we could find patients easily that would most obviously be a candidate for these services, which gets me back to the point earlier about the home and community-based waiver patients, would there be a way to flag these patients? So, the Medicare part D plan would know they were a waiver patient who required this higher level of care in the home. And that would just be one seemingly, easy target, right? To say those patients should be eligible for these services. I would say that we don't have the perfect answer yet, nor that there will be ever a perfect answer, but we definitely have some guideposts that we've been discussing.
Todd Eury: It is almost like coming up with a home care certification. And now if you pass, you're a community pharmacy, if you go do this, I don't know who's going to control it - CMS or something. Or, if you fill out this application and you fit, the services that we require you to be able be able to deliver just a very small percentage would need an IV. But, if you have the ability to deliver that, even with partnerships, now you become a certified home care pharmacy. Susan, is that the way to go about this? Come out with some kind of certification that assures the paying entity that they're able to deliver those specific services?
Susan Rhodus: Actually, that piece of it technically is already there because CMS has a list of 10 criteria, which include two regarding that emergency kit, which we would knock those out. So, you're talking about eight different criteria that they have to follow. And in order to belong to a long-term care network, you have to sign off saying that you're able to do those criteria that are on that list. So, if you can't do those and you don't sign up for the network, then you're not in the network. If you sign up for them, then you're in. So, it's not super difficult to do that if you're able to do all those things. And again, those things that are most important on that list are, you know, delivering medications, the packaging of the medications, the 24/7 availability of the pharmacy and the pharmacist.
Those are all the things that are really important to make sure that you can do. If you can't do those things, then you really don't qualify. And then we're talking about being able to do other services as well. Like we talked about medication management, reconciliation, the syncing of the meds, which a lot of community pharmacies are already doing. So there really aren't a lot of extra things they would need to do. They would need to be qualified as a long-term care pharmacy to qualify. Now the patients are another dilemma - it really needs to be national criteria because otherwise we're in big trouble. We could have a different one for every PBM that's out there. And if we had different ones for every PBM, we would have an absolute nightmare for the pharmacist to determine what they have to fill out for which Part D plan.
So, I think that having a national basis to determine those criteria is going be really important. And like Ronna said, we are in the middle of discussing that right now, but things like needing help with two ADLs, which is activities of daily living per day, things like toileting, dressing, feeding, taking medications, getting transportation to go get things like groceries, keeping your house maintained, things like cleaning your house - those types of things are all parts of those activities of daily living. And usually to get into a facility, you have to have issues with two of those or more. Most people who are in a nursing home probably have more than that. I mean the number one reason to go in a nursing home is that you're incontinent. So that's the kind of thing that people look at to get institutionalized. And then things like you’re home bound, you can't leave your home without having someone assist you. So, those are the kind of things that are going to be really important on that list. And I think that's an ongoing thing. Like Ronna says, we're never going to have a perfect list, but we can definitely work at it to have something that the government can say, yes, we agree with this.
Todd Eury: So, we're talking about long term care services that are being now injected into the home and being delivered by community pharmacy. And there's a blending of that firewall between community pharmacy and long-term care.
With 71 million baby boomers, we know that community pharmacies have to be ready, prepared, and also get paid for the services that they can deliver to these home bound patients that don't want move out of their home.
There are no facilities to take them in or give them a bed anyway. So, talk to me about your experience as a pharmacy owner and what you're doing for those patients and the navigation of the beast, which is, “Hey, we’ve got to get our pharmacies paid to deliver these services.”
Joe Williams: You kind of hit the nail in your head when you reference the baby boomer. You know that generation that we're going through now is one of the largest generations to have ever lived. And they're at an age now where they're kind of at that tipping point of what's going to happen next to them. I know that my parents and I have had this conversation and they're pretty adamant that they never want to be placed into a facility. But you know, I'm like so many other people now that I have a busy lifestyle myself, I work probably way more than I should. So, the idea of me being able to constantly care for my parents around the clock is not really the best plan. And so, trying to keep them at home or keep them in a private home, you've got to look for ways to close some of the gaps that they may be dealing with.
So, a couple years ago, we came up with a program called MedSmart that was intended to fill and close some of these gaps. Originally, it was intended just for our general population where we are in Southeastern North Carolina, where we discovered that the biggest concerns and issues that most patients faced were lack of transportation and medication non-compliance.
So, we started building this program to really solve those two problems with free deliveries, free compliance packaging, and then a more intimate relationship with the patient and the providers that were prescribing their medications.
And what we found as we started doing this is that there was a huge demand for this, not only with transitional care patients who were leaving the hospital, where we were receiving referrals from those hospital systems, “Hey, help us keep these patients out,” but also amongst geriatric providers themselves.
And then, and I think this is going to help with what Susan and Ronna were discussing. We were getting a lot of referrals from home health agencies. So again, the kind of folks that I would probably be talking with when my parents are remaining in the home, someone that can go by and help them with their ADLs, you know, those activities of daily living. Kind of help to provide them with the additional support that they need. And these services are available on a commercial basis. They're paid by some payers depending on what's going on in the patient's life, but there's also a lot of those that do private pay as well.
And so having a relationship with those kinds of folks that are going out and helping this particular patient population opened our eyes up to the need for this to expand just beyond your traditional physician referral or your traditional hospital discharge referral.
And the great thing about like what Susan's mentioned that there are certain obligations that we have as providers to make sure that we're doing everything the right way. And she pointed out that two ADL list, well, nine times out of 10, if they're being cared for by some of these home health agencies, those ADLs are already there. There's that demand. And you're simply going to make that patient's life easier. And for that matter, you're going to make the job of that person who's helping them with those ADLs, that much easier. Because a lot of times the medication compliance piece is something that they struggle with as well.
Todd Eury: Talk to us about your organization, Joe, and your home care services and, and how you're navigating that to ensure that you're getting paid.
Joe Williams: So originally when we started out, um, we, it all started with one patient and, we originally started with multi-dose blisters because there were no barriers to entry. It was very inexpensive to jump into. And we were really caught off guard by the demand.
So, we grew so fast that the rate limiting step was what our pharmacists were capable of checking. I had four or five techs that were assembling multi-dose blisters around the clock, and they could fly through them. They would do a fantastic job and, and there were with little to no errors. There would be occasionally human error, but then as the pharmacist, I would have stacks on my counters of all these compliance packaging, and we went through every single sale.
And so, we were just getting really bogged down and we started looking for solutions that because for most things to be successful, they have to be scalable. You know, you have to be able to continue to provide the service and you have to either, you have to either really be super intense in a specific region, or you have to expand that region to give you what you need. And so, we actually have expanded at this point to nine counties in Southeastern North Carolina and the solution that allowed us to do that was the RxSafe RapidPak.
We've experienced massive flooding, hurricanes — all of these things. And we can proudly say that no patient has ever missed a dose because of us. We've done everything to make sure that they had it.
—Joe Williams, Brisson Drugs Owner and Pharmacy Consultant
We found that once we kind of capped out with multi-dose blister, that we needed a better solution, we really needed a way that we could streamline the check process, the verification process, and the RxSafe has been the system that we found has been the best for us to do that. Beyond that, it was a matter of transportation. It was a matter of having a plan. If you've ever heard me talk about our delivery model, we began with the end in mind, like I knew five years ago that I was going be covering Southeastern North Carolina. And we started building a delivery model that was going to accommodate one day, and then we allowed ourselves to grow into it, keeping those necessary efficiencies in mind so that it was going be scalable long term.
Some of the biggest obstacles that most owners face is having a streamlined process for acquiring the patients, getting the packaging done in a timely fashion, and then being able to get that back out to those patients and in a reasonable amount of time, because once you take them on as compliance packaging patient, at least this is how it is in my store, I take responsibility that their next dose, their next time dose is never, ever going to be late. We've experienced massive flooding, hurricanes - all of these things. And we can proudly say that no patient has ever missed a dose because of us. We've done everything to make sure that they had it.
So, you really have to kind of be prepared for the unforeseen. You have to be prepared for more demand than you expect to be there. And then you have to be available to those patients because you're going find that when it comes to your patients who are in these programs, you become a lot more intimately involved with them than you do some of the patients that you may only see every 30 or 90 days that are walking in your store on sync, because you, you are taking responsibility for every dose, every med pass time, everything, but that's what we want as independent pharmacies. We want to be connected to our patients, and it's a beautiful way to do it.
To listen to the whole discussion, click here.
To learn more about how you can move into the LTC space through GeriMed’s ComboMed program, click here to contact us or speak with our pharmacy transformation experts at (833) 791-1772.

.png)