Long-term care at home empowers pharmacies to deliver proactive, personalized care where patients need it most. With new reimbursement models and the right technology, independent pharmacies can scale services, support vulnerable populations, and turn essential care into sustainable growth.
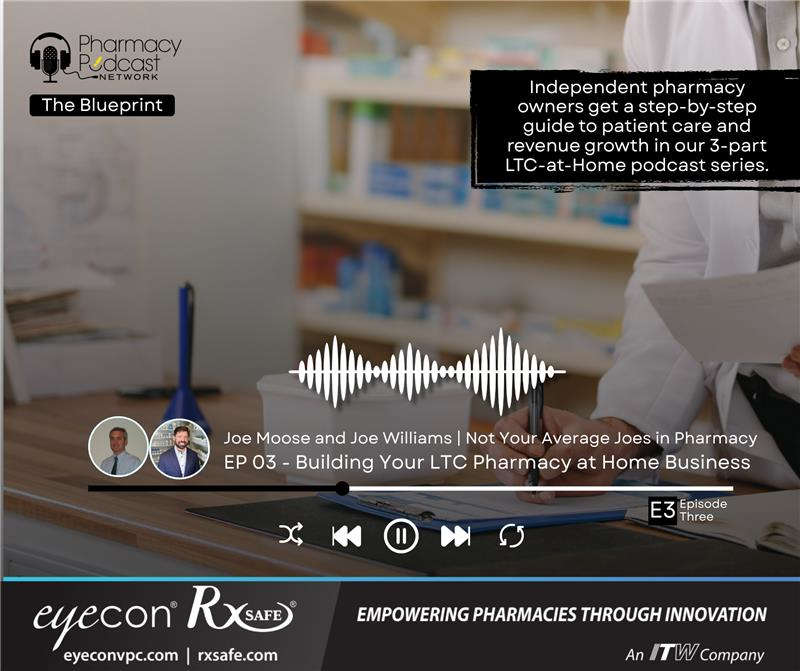
In the final part of the Pharmacy Podcast Network’s LTC@Home series, “Not Your Average Joes, LTC Pharmacy at Home”, Joe Moose and Joe Williams give expert advice and actionable strategies for pharmacies that find themselves struggling to keep up with patient demands.
Featured guests were:
- Joe Moose, Lead Community Pharmacy Coordinator & Owner of Moose Pharmacy
- Joe Williams, Pharmacy Owner & Operations Consultant at Apex Pharmacy Consulting
Below are some podcast highlights. The transcript has been edited for clarity and length.
Todd Eury: We're going to be concentrating on the concept of long-term care pharmacy at home. What does that mean for our community? Independent community pharmacies? What does that mean for the expansion of community pharmacies throughout the nation? And to slow down what we know is happening—which is the increasing of pharmacy deserts throughout the nation. We do not have enough pharmacists' services and pharmacy services including this very specific topic of today, of long-term care pharmacy. And I really want to give a shout out to Eyecon RxSafe for helping us collect information and great guests and people who know what it's like to expand these services from what you did back in the day. I'm old enough to say that now where I've been around pharmacy since 2004, and I remember when community Pharmacy was doing assisted living. They were doing services to long-term care, but they weren't getting paid for specific things that they were doing. And now we have mechanisms through CMS and through reimbursement to ensure that you are getting paid for services that you're providing, that the people in your communities desperately need. And I just want to give a shout out to our guest today. I want to start with Joe Williams being part of this discussion today and for being a service to other owners through Apex Pharmacy Consulting.
"We were smart enough to grab that RapidPak--we were number 17, I think, to install—we were smart enough to get it onboarded early on. And then last year we doubled it in capacity. We added 20 additional slots so that we could go to 40 slots. And we think now that we can do more than a thousand patients a month just in packaging out of that one machine. And this is the funniest part, it's where a refrigerator was. I didn't tear down a wall, I didn't build an extra room. I didn't buy the adjoining property. I moved a refrigerator, and I put a RapidPak there, and then I won back the entire back half of my pharmacy that was used for filling blister packages. So yeah, it's kind of a no brainer how this thing works."
- Joe Williams, on how the RapidPak allowed him to grow his practice.
Joe Williams: Thanks, Todd. I appreciate you allowing me to be here today.
Todd Eury: And Joe Moose with Moose Pharmacy—just a beacon of evolution and how you've leveled up your community pharmacies and the extension of long-term care at home through Moose Pharmacy. Thank you for being here, Joe.
Joe Moose: Thanks, Todd. Great honor.
Todd Eury: I have to reference an article that came out in McKnights Long-Term Care News and the title of this article was “Bill would designate pharmacists as providers, allow reimbursement for more LTC services” and this goes through legislation that would enable and empower long-term care pharmacists to bill for more of their services that they're already providing, ensuring community access to Pharmacy Services Act or known as ECAPS, which was introduced way back in May of 2025. This is relevant, this is important, and like I said in the opening, we have to slow down what's happening to our nation's services. I do want to start out just with someone who's experienced the growth and the transformation from being specifically a retail-oriented community pharmacy and expanding into long-term care. I'm going to kick this off initially with Mr. Joe Moose—and excited to have you here, like I said, Joe with Moose Pharmacy.
Joe Moose: Yeah, I mean we have always had one compass—and that was take care of the people in the community we serve. And it doesn't matter where they happen to be, you may be taking care of them at work, you may be taking care of them at home, or they may go into some type of facility. So, I think that the new buzz is this term long-term care at home—but it's really what we've done for years: taking care of people at home. And it's a lot less about filling the prescription and the transaction of getting the prescription to a patient and a lot more about helping the outcome of the patient. This whole idea of taking care of a patient in their home, letting them stay where the most affordable healthcare is—is in the home and not in a hospital or not in a facility
So doing whatever it takes to allow that individual to stay in the home, then I think this just naturally makes sense. And the progression from that was not an overnight decision. It was an overnight decision to invest in the RxSafe and to use packaging, but it’s been a day one decision—back in 1882 when my great grandfather started Moose Pharmacy—was to take care of the people in that community. So, how we do it has changed a little over the years, but that's still always been the compass.
Todd Eury: I appreciate that and that's absolutely what we believe in—just taking people and understanding how they're transitioning in life—and we're all getting older. Joe, you are, through Apex Pharmacy Consulting, helping other community pharmacies implement services as well as strategies that go even far beyond long-term care at home. But let's dial into that topic and how this has impacted your own pharmacies throughout the years.
Joe Williams: The way that we found ourselves in LTC at home, it's kind of like what Joe said. We started with packaging—and I have a story that I tell a lot about for one patient that really needed it—and that was so productive and so helpful for that one patient that we just continued to expand that service to more and more people.
Well, eventually we found ourselves in a place where—from a manpower standpoint—we just couldn't keep up anymore. We didn't have enough counter space for packaging bubble packs manually. I did not have the time in my work week to be able to verify everything. And so we looked for a solution and we discovered the RxSafe RapidPak and we were able to win back so much time—in both in packaging and verification—that we continued to scale.
When LTC at home came along, we didn't have to launch this big marketing program. Those patients were already in our pharmacy, they were already in packaging, they were already qualified. It was as simple as making some software changes to go ahead and be actually reimbursed more fairly for the level of effort that we were providing to care for all of them. In our market, we are in a very low income area as most know about me, and we're not able to charge people for packaging, we're not able to charge people for delivery—at least we don't feel like we can. And when the opportunity to place so many of those patients in LTC style plans and actually reap the benefits of the level of effort that we were providing, it was a major windfall for our stores, that's for sure.
Todd Eury: Joe Moose, Moose Pharmacy, I want to—just in case our listeners don't understand or kind of can't track this—because it's funny how you're not getting paid for something that you've been providing for such a long time. You made reference to the late 1800s when your family's business started and you always delivered what the patient needed. Now we're evolving, now it has to be officiated. Now if CMS is going to be reimbursing these things, can you kind of give us an idea of what the technical parts are of this? I'm thinking of targeting medically complex patients, I'm thinking of specialized packaging, 24/7 ability to give clinical or emergency access support. Obviously, this referral network—the network and the right way of billing. And then just understanding: How does that service the individual patient that has no family looking after them, they have no delivery capabilities? Give us an idea of: What are the parts of this puzzle?
Joe Moose: Yeah, it definitely is a workflow change, Todd. So, it's care coordination at its most core behavior. So to do that, it is not about filling a prescription fast, accurately and cheap. It's not a transactional thing. We connect with the patient, we do it telephonically and face-to-face. It's being very proactive. So, kind of our workflow is: We start out, if somebody is already in our program, we're starting out seven to ten days before we know they're going to need their medication. We're calling them, we're checking in, we're asking about things like have you been hospitalized? Have you gone to the doctor? Has the doctor changed anything? What type of outcomes? If they're on medications for diabetes, what type of blood sugar readings are you getting? If they're on a continuous glucose monitor and we're monitoring that for them, we're reviewing that with them. So, we're working on this patient throughout the month and we're anchored around this one care planning, care coordination phone call. It requires documentation of what's going on in that phone call because we've got multiple people touching this patient.
We've got technicians, we've got pharmacists, we've got community health workers, we've got delivery drivers. So multiple people are touching the patients and getting information from that patient. So it's got to land in someplace where anybody who's touching can see what somebody else has done. So we use care plan as a documentation platform for that, and then it's coordination. We're all singing from the same hymnal, here's what we're trying to do. So we're sending it to our RxSafe for packaging on it. When it comes back, we're marrying that up with the meds that don't get packed like inhalers, or nasal sprays, or topical ointments, those types of things. And then that's going out to the patient in their home setting. At the time that they're going out, there may be a community health worker that's going out there and doing some type of assessment of blood pressure.
We're documenting those recordings of what those readings are, and then we're connecting with the physician to say, “Hey, here's a drug therapy discrepancy. Or here's where we think therapy may not be being optimized and the patient's blood pressure is not at goal on it.”. So, it is an orchestra going on to try to deliver a great concert that the patient benefits from. And so, it certainly is this whole idea of pharmacy care at home. I think that the term “long-term care at home” is sort of a misnomer—at least a confusing nomer—that everybody associates with something going on in a nursing home where this just gets down to, like Joe said, good old fashioned taking care of a patient. So, if your goal is to take care of the patient in the end, you quit focusing on one drug and filling that one drug and you start focusing on the things that get them outcomes. And sometimes that's social determinants of health, sometimes adherence and how well a patient's doing in adherence, and how you can coach them through that. Sometimes that's being a cheerleader and sometimes you're the only person that that patient is really talking to in terms of healthcare journey. So, you're doing a lot of coaching coordination of that care and then keeping them accountable for actually following the care plan.
Todd Eury: Joe Williams, I want to flip it for just a second because when I'm listening to Joe Moose speak on this and kind of breaking it down, it's making sense. However, I like to understand from a pharmacy owner's perspective, what's keeping us from pulling this lever and in keeping us from going to that next level and making sure that we have the documentation, that we have the right processes, that we've implemented the right technology—in this case, the Eyecon RxSafe technology. So, break it down for us from a pharmacy owner's perspective. I am not a pharmacist, I am not a pharmacy owner, so I want listeners to understand things from the other side. So, you're dealing with this as a consultant, helping community pharmacies get through this. So, share with us some of those stories of what's holding them back.
Joe Williams: That's a great question. What separates a lot of pharmacy owners from the “Joe Mooses” of the world is what you're getting at here. And I give Joe a lot of credit. I've been to his stores, and they do a fantastic job of coordinating so many different things like he's talking about versus—and I'm not talking about anybody in particular—but I go into a lot of other pharmacies and it looks like the pharmacist is juggling burning cats. And so, what happens nine times out of ten—and your typical pharmacy, your typical independent pharmacy in this country is you have a pharmacist in there that loves their community, that loves their patient, that loves their staff, that is doing everything in their minds humanly possible in that moment right then to take care of everybody to the point that they don't have any freedom to take those two to three steps back, look at the total operation and figure out how they're going to start moving forward with all of the things that they would really like to do.
And so, one of the things that when I'm starting to help someone and they're asking me what all of their problems are, I'm like, “Well just stop for a second. Just plant your feet and back up and look here. You can continue to run on this wheel like a hamster every day and exhaust yourself and just praying that Saturday at one o'clock gets here as quickly as possible, or you can back up and start to get a game plan together.” And so, is the holdup that you don't the marketing to attract the type of patient? Is that you don't have the physician relationships to be able to give you the referrals? Is it that you don't know who any of the home healthcare entities in your marketplace are? So, figure out what the problem is.
Now, there is somewhat of a question depending on your mindset of the chicken and the egg. So there are those out there that feel like they need to develop a program that is as extensive as one that I have or that one of the other Joe's has. They feel like they have to build this entire program in the backend behind the curtain. They have to have everything ready. And then one day, like you said, they're just going to pull the lever and the machine is going to turn on. That's not the only way to go. I mean there are those that do that, but Joe's probably like me. Joe probably started doing things and started growing and started helping people and then said, okay, now it's logical that we need to add in this technology.
Maybe it is okay to start and get X number of patients into packaging, and then you're manually packing and you're getting a feel for it. You're figuring out your processes, you're creating workflows, you're creating your champions and specialists. You're determining how you're going to be coordinating all of this. And then you go ahead and you get the ball rolling. So like I said, it's chicken or egg. It's based on your philosophy of business and your philosophy of operation. But the biggest thing is, is you got to start going in that direction. You got to get off the hamster wheel running as fast as you can remaining in the same place and start setting some goals for yourself.
It's going to be this number of patients, it's going to be this number of marketing calls, it's going to be this or that or that. And it's really not that hard, honestly, it's not. Once you start rolling. Listening to Joe, it's like I'm standing in one of my stores. We won't even start a patient on packaging until we've gone to their house and gone through their medicine cabinets. We go to their house too. Just same way. I want you to have a relationship with us. I am not a store on the corner that is a vending machine for drugs. I have a lot of licensed healthcare professionals that are here to take your expectations—your health comes to another level. So, let me help you, and then having—and Joe said it better than I'll ever say it—but just having that big picture mentality about how you're going to do these things. And so, just start. Start going down the road and before you know it, you'll become more efficient because you'll be doing it more and more and then you'll start winning back time. You'll be able to bring on extra staff to help you with these things because of the return on the existing patients that you have. And then one day, you'll do like me and you'll just be trying to be more and more like Joe Moose.
Todd Eury: I love it. I love it. It goes back to what Joe Williams was saying about implementing and following up, being consistent. Joe Williams, you are out there talking with pharmacy owners. There's going to be questions that they're going to have. There's going to be listeners right now, are they going to have these questions? One of the first questions is, so how many patients am I already taking care of that if I just did the right proper paperwork, if I did the right proper procedures, if I had the right technology, I could backfill with 40, 60, 80 patients that I'm already struggling with to deliver true long-term care or care services at the home. So, talk to us about numbers and what we should be thinking about as pharmacy owners.
Joe Williams: So, good question. The biggest thing—numbers are important—but the big thing is having clean data, I think out of the gate. We help a lot of pharmacies at Apex, Ben and I, with a lot of third party cleanup information. Unfortunately, not everyone begins with the end in mind when it comes to organizing their third parties and placing patients into the correct ones. But, if someone had organized third party data and they could easily define how many patients they had and Express Scripts Medicare, how many patients that they had in UnitedHealthcare, Medicare, et cetera, it's not complicated to determine what your lift would be by getting into a packaging program, acquiring a machine from RxSafe and getting started with it, combining that with an LTC at home contract. Number wise, the old number that we would openly use regarding more of a breakeven mentality, if you will, is about 50 patients in packaging. But you have to realize that those numbers were based on retail contracts at the time. So, if you're looking at it from an LTC at home contract perspective, that number is much lower. I don't know the math off the top of my head as far as what that count would be, but I will say that if you think big picture and you initiate these things together—the LTC at home combined with the machine, the RxSafe RapidPak—you are far lower than 50. Now.
And the delta between what you see on your screens in traditional retail and what you see in an LTC at home contract—it's almost unsettling. It can be so different. I mean, when you see the benefits of ensuring that the patients are enrolled in the best plans for themselves, ensuring that you have an LTC billing MPI to make sure that you are following the rules, and you're doing everything right, and you can do all of this. There's consultants out there that help you. The good folks with GeriMed with Eyecon RxSafe can help you do this. There are so many different add-ons. And just by organizing that data to begin with, it also offers and creates a lot more opportunities long-term as far as additional benefits of dispensing, additional benefits of patient care add-on programs that are specific to certain payers. It's that big picture thinking. Again, and this is just one big piece of it by having them in packaging to make sure that you fulfill those obligations of LTC at home.
Todd Eury: Yeah, I like the tools that are provided by the Eyecon RxSafe team because one of the tools is a preface—and that is, they're going to take you through an exercise and they're going to marry in some of their consultant teams to be able to be like, “Okay, let's assess how many patients are you already working with so that when you hit the ground running, there's reimbursement coming in because we filled out the forms, we got enrolled, we're truly doing long-term care at home, we're making sure that we're compliant.” and therefore, from that infrastructure—that base—now you get to just build your business and get to add in some other things like the clinical services that Joe Moose was talking about, fold that against your CPSN directives and blueprint because there's a bigger game here so that we're proving things to the states, but we also want to be proving—continue to prove things to federal level CMS, that “Hey, when we're implementing long-term care services at the home, it's going to save our entire healthcare system, emergency room entries and not getting your right medication and waste.”
How many times we send through mail order these big packs of medications that set unopened, and they expire or something like. So, all this interaction with the patient goes far beyond just the medication management. It's also the engagement like Joe Moose was saying from the beginning of the late 1800s of really caring for that individualized patient's needs. And in many cases, these people don't have any support. They have family that might live far away, or they don't have somebody visiting, or they don't have somebody just doing a checkup.
I want to talk about data and Joe Williams, that's important to you and the expansion of your consultancy business because you're standing behind the blueprint that you're helping a pharmacy implement. Part of that is the data—being able to show, here's the benefit. The data for me in this question to you is about the audit—the dreaded audit that may happen someday. Well, if you're following this process and you're assuring your own systems and you're assuring your tech partners like Eyecon RxSafe, you're ensuring the expansion of your business and your communities that you're compliant. But talk to me about data in audit prevention by being a good steward of data.
Joe Williams: Yeah, no, absolutely. Absolutely. Given that we use the RxSafe and the Eyecons, I mean we're down to the lot number on our fields now through the QR codes on their devices, using it in our fill stations. We have images of every single pill. Literally every single pill that walked out of our store, whether it was taken before it was placed in the RapidPak or whether it is—while it is packaged in a patient's package, we have signature logs from everything that was picked up for the patients. We have copies of their MARs and medical records from their physician practice from when we enrolled them to the program to ensure that their med list—as provided by the other pharmacy or by the patient themselves—is accurate. The level of depth of information and data that we have on a patient that is in our RapidPak program—the Med Smart program is what we call it in our stores—I mean, I only wish that the rest of my patient population was as detailed.
There is a significant portion of the prescriptions that we dispense that are “fast, accurate, and cheap” as Joe described, and that's the case in any, well in most pharmacies. But when it comes to those patients that are in the Med Smart program, we’re delivering 99% of those to the home. So we have recorded call logs from where we've talked to the patient, as many of them as possible are enrolled in chronic care management through their physicians because we have a partnering CCM program with those physicians. So, we have another team that is contacting them at home and spending time with them each month. They really legitimately feel like they have personal relationships with our entire team. This is not like some patient populations that may be deemed “profitable” by some pharmacies, but the pharmacy doesn't enjoy dealing with those patients. These patients are patients that need us. It's rewarding work. We're improving their outcomes. We're helping them at every turn. And Joe, you led the way. You and your family have been around in this business for a long time and you've been steering some of these things. We are starting to see changes. Just recently, UnitedHealthcare, a major payer, just dropped actions for us into the EQUIP dashboard at my stores where we're being asked to collect blood pressures, A1Cs. It's taken a long time. I mean, the Asheville Project was so many years ago, and you would think this would be occurring in every pharmacy today, but I know in our pharmacies, we are building in-store care actions to execute these things already. And so many of those actions are actually for bedbound patients that are in the Med Smart program. And we're sending our staff into their homes to collect blood pressures, to collect A1Cs. I mean, we are an extension of the physician practice, we're an extension of the carrier, we're saving the PBMs money. So, when I'm standing in front of—and I've had to do this this year quite a bit—when I'm standing in front of five or six lobbyists arguing about pharmacy reimbursement, I'm able to tie in the benefits of what we're doing in our programs. And I couldn't do this at scale to make it significant enough without having the right technology in the store to free me up to do these things. If I was still packing blister packs on the floor, on the wall, or on every counter in there and I was spending all afternoon until nine o'clock, and then every day, all day on Sunday checking these things, there's no way I could be standing in the general assembly building in Raleigh arguing with the PBM lobbyist.
We were smart enough to grab that RapidPak-- we were number 17, I think, to install—we were smart enough to get it onboarded early on. And then last year we doubled it in capacity. We added 20 additional slots so that we could go to 40 slots. And we think now that we can do more than a thousand patients a month just in packaging out of that one machine. And this is the funniest part, it's where a refrigerator was. I didn't tear down a wall, I didn't build an extra room. I didn't buy the adjoining property. I moved a refrigerator, and I put a RapidPak there, and then I won back the entire back half of my pharmacy that was used for filling blister packages. So yeah, it's kind of a no brainer how this thing works. And half the time now, I just find myself trying to get out of my own way and let it keep going and growing.
Todd Eury: Love it. Well, this topic is important. It's going to continue to be discussed at a national level. I just want to say thank you to organizations like the Senior Care Pharmacy Coalition, who is out there advocating to continue to push long-term care reimbursement into the community pharmacies—independent community pharmacies. And shout out to partners like Eyecon RxSafe for being here and waiting to hear from the Joe Mooses of the world, and the Joe Buntings of the world, and the Joe Williams of the world asking you, “How can we make this better? How can we keep up? How can we keep pushing?”.

.png)